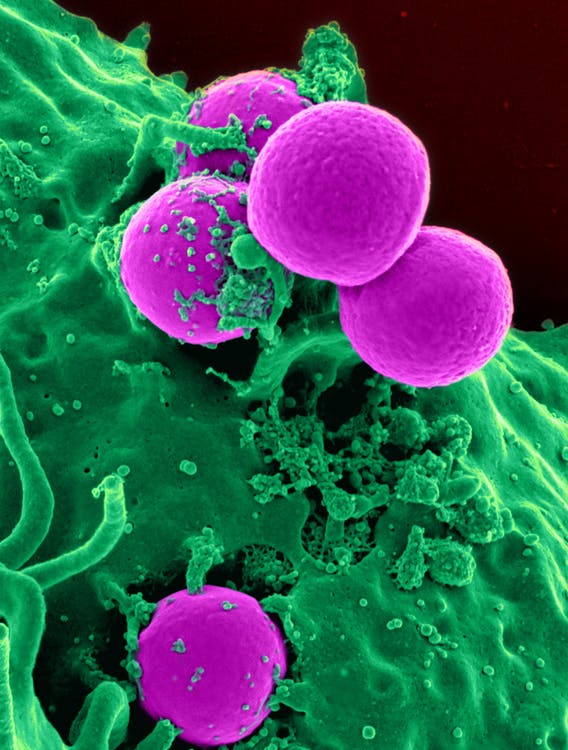
Generally speaking, your immune system keeps you safe from infectious diseases and illnesses. It produces certain cells that are meant to attack foreign cells when it detects these types of pathogens. This is due to the capacity of the immune system to distinguish between cells in the body as well as know which ones are harmful and which are beneficial.
Though the majority of individuals associate disease with viruses and bacteria, these illnesses can sometimes result from the body’s natural defenses working against them. However, if you suffer from an autoimmune condition, your immune system mistakenly views your skin and joints as indifferent parts. Thus, proteins released by the body, known as autoantibodies, target healthy cells.
The body’s immune system can be just as harmful to other entities as it is to its own tissues. Individuals with an overactive immune system frequently experience many autoimmune diseases concurrently, causing destruction in their bodies. Common examples include rheumatoid arthritis and multiple sclerosis, which affect the joints and myelin sheath, respectively.
Certain autoimmune illnesses are limited to a single organ, just nerve cells, blood vessels, or other organs. The digestive system is harmed by type 1 diabetes. Some illnesses can impact your whole body, such as systemic lupus erythematosus or lupus.

What Can Cause Autoimmune Disease?
Experts and professionals are unsure of the precise origin of immune system malfunctions. However, there are individuals who are more susceptible than others to developing an autoimmune disease. The following are a few variables that could make you more susceptible to getting an autoimmune disease:
Gender
Between the ages of 15 and 44, those who had been given the gender of female at birth had a higher risk of developing an autoimmune disease compared to those who were born male. This is because autoimmune conditions are more common in women than in men, but illnesses that are infectious affect them less frequently. The X chromosome, which contains numerous genes connected to the immune system, may be partially responsible for this increased frequency.
Genetics
Genes that are inherited may increase your risk of developing autoimmune illnesses, while factors in the environment may also play a role. You’re more vulnerable if there is a history of autoimmune disorders in your family because some of them run in families. Additionally, autoimmune illnesses may potentially be more common in people with specific genes. Genes contribute, but they are insufficient in and of themselves to produce an autoimmune illness.
Environmental Factors
An increased risk of autoimmune illness may result from exposure to sunlight, the element mercury, compounds used in farming, tobacco smoke, and some viruses and bacterial infections, among other things. Microbes such as bacteria and viruses have the ability to cause alterations in your immune system that cause it to fight against itself. It may be more likely to occur if you have a hereditary predisposition to immune system disorders.
Nutrition
The nutrition and food you eat can affect the likelihood and seriousness of autoimmune illnesses. Ingredients in food have the power to influence how the immune system functions in an anti- or pro-inflammatory manner, either directly or indirectly. While any dietary shortfall can occur, some of the most frequently associated with nutritional deficiencies with autoimmunity are those involving minerals such as magnesium, zinc, vitamin A, vitamin D, and omega-3 fatty acids.
Medication
Certain medications may alter the way your body functions through processes that affect your immune system. Particularly, you should discuss with your medical professional the adverse effects of antibiotics, blood pressure drugs, and statins. Add the list of medications to the ones you will question your healthcare provider about, such as hydrochlorothiazide, antithyroid, sulfasalazine, penicillamine, terbinafine, anticonvulsants, and fluorouracil agents.
Other Health Conditions
You may be more susceptible to developing an autoimmune disease if you have certain medical problems, such as obesity, along with other autoimmune disorders. Even with a good diet and regular physical activity, an obese person’s body’s defenses may nevertheless weaken. Certain research has demonstrated that obesity itself reduces immunity.

Numerous other autoimmune diseases also have a significant negative impact on your health. We’ll look at the most common and rare autoimmune disease examples here that you must be aware of.
Uveitis
When the eye becomes swollen and inflamed, it is called uveitis. The body’s reaction to an infection or health problem is inflammation. The majority of uveitis instances are associated with a breakdown in the immune system (the physical defense against illness and sickness). However, rarely, uveitis can occur without causing swelling or redness in the eye.
An uncommon autoimmune condition known as uveitis results in inflammation or swelling of the optic nerve, the gel-like substance that provides the eye with its shape—the vitreous—and the darker layer of the lens of the eye, known as the uvea. The typical treatments for uveitis include intravenous, anti-inflammatory topical, and corticosteroids taken by mouth. Note that there might be a cause of discomfort and infection in the eyes.
Psoriasis
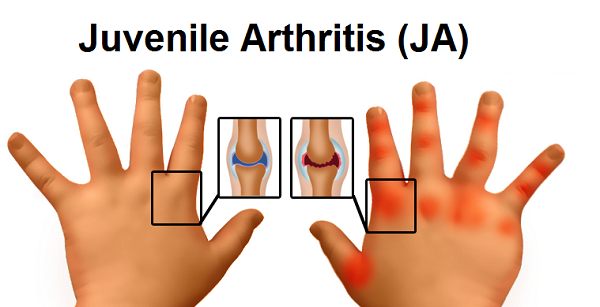
Psoriasis is a chronic skin condition that is caused by an autoimmune disorder. It is marked by red, elevated, swollen, inflammatory patches on the scalp, knees, elbows, and back area that frequently turn into silver-colored scales. That is because the T lymphocytes, a subset of white blood cells, wrongly target the skin cells.
Psoriasis and other dermatological disorders are sometimes misunderstood to just cause cosmetic discomfort. However, during illness flare-ups and episodes, injuries to the skin can become extremely serious, much like in the case of those suffering from burns. Because of their inability to control their body temperature, people with psoriasis are more susceptible to infections that might prove fatal.
Grave’s Disease
Hormonal abnormalities can result from thyroid gland inflammation, which is brought on by a variety of uncommon autoimmune disorders. Antibodies cause the body’s thyroid gland to produce excessive amounts of thyroid hormone, which can cause red skin, shaking hands, and irregular heartbeats. It is what causes Grave’s disease.
Graves’ illness impacts multiple facets of your health. Exophthalmos, or swollen eyes, higher energy levels, heat intolerance, problems sleeping, vomiting and diarrhea, and anxiety are characteristics of the illness.
Sarcoidosis
An autoimmune-related condition called sarcoidosis results in the accumulation of inflammatory cells that affect particular connective tissue in the body, most commonly the skin, lymph nodes, or lungs. Granulomas are the small, grain-like lumps that are the beginning of it. Each of the organs in the body may be impacted by it.
Although the exact cause of sarcoidosis is unknown, the autoimmune disease’s symptoms, which include skin lumps and dyspnea, can occasionally result in arrhythmia or an abnormal heartbeat when other parts of the body are damaged.
Vitiligo
Many times, vitiligo is confused with hyperpigmentation of the complexion of the skin. On the other hand, vitiligo is an autoimmune disease that is chronic (persistent) and results in areas of skin losing their color. The outermost layer of the skin turns a milky-white tone. These are from the attacks of healthy cells causing the destruction of melanocytes, the skin cells that produce colored pigment.
Patchy disappearance of skin pigment, which typically starts on the hands, the face, and around bodily openings, including the genitalia, is one of the early indications of the autoimmune disease. Premature graying or whitening of your eyebrows, beard, eyelashes, or scalp hair, as well as the discoloration of the tissues lining the lining of the nose and mouth.
Addison’s
The hormone release system, the endocrine system, is impacted by Addison’s disease. If the immune response targets the glands that produce adrenaline and seriously harms your adrenal cortex, it may manifest. The hormones cortisol and adrenaline, both of which sustain the body’s and its organs’ ability to produce energy, are insufficient when the adrenal glands are injured.
Many symptoms may result from this, such as discomfort, impairment, low blood pressure (caused by salt loss), and skin discoloration in some places. Acute episodes can also result from low levels of hormones, which raises the risk of coronary artery disease, lung problems, weight gain or obesity, stress, depressive disorders, and other illnesses.
Pernicious Anemia
Pernicious anemia is a type of vitamin B12 deficiency anemia. It occurs when the body lacks enough healthy red blood cells due to an insufficient amount of vitamin B12. This deficiency often results from the stomach’s inability to properly absorb vitamin B12, frequently due to a lack of intrinsic factor—a protein necessary for vitamin B12 absorption. Common symptoms include fatigue, weakness, memory loss, and neurological changes.
Giant Cell Myocarditis
Giant cell myocarditis is a rare and often fatal type of inflammatory heart disease characterized by the presence of multinucleated giant cells (cells with more than one nucleus) in the heart muscle. It is a severe form of myocarditis, leading to rapid deterioration of cardiac function, and can result in heart failure or sudden death.
Vasculitis
Vasculitis refers to a group of disorders that involve inflammation of the blood vessels. The inflammation can affect arteries, veins, and capillaries, causing them to narrow, weaken, thicken, or scar. This can reduce blood flow and lead to organ and tissue damage. There are many types of vasculitis, and they may vary significantly in terms of which organs are affected, the severity of the condition, and the symptoms, which might include fever, fatigue, weight loss, and muscle pain.

Treatment Options for Autoimmune Diseases
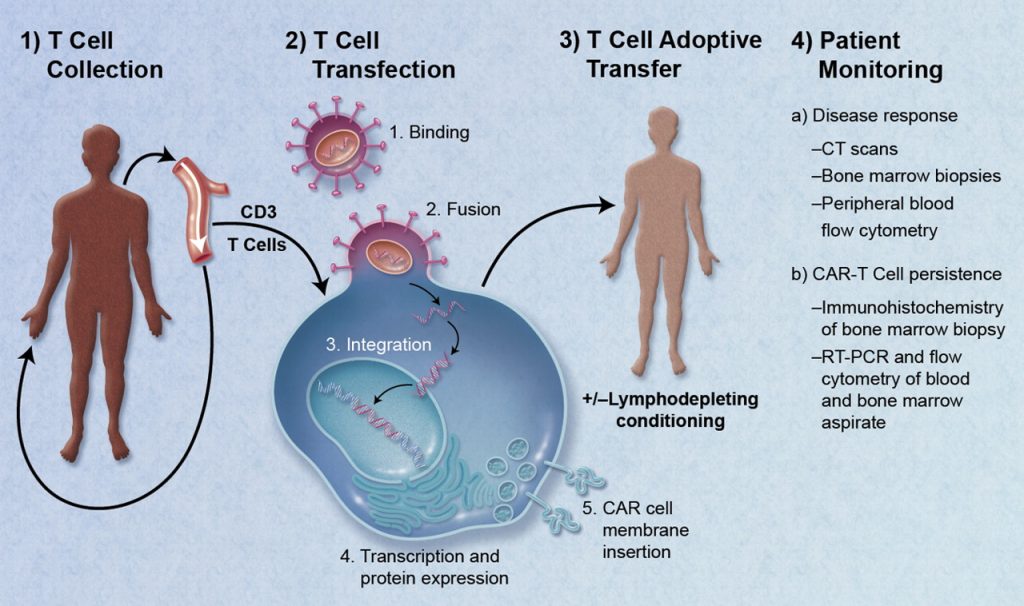
Normally, the immune system’s mechanism creates antibodies that are intended to fight off a particular infection, bacteria, or other foreign material. However, this is not the case with autoimmune diseases. Although autoimmune illnesses currently have no known remedy, there are numerous therapeutic options that can help alleviate your symptoms (pain, fatigue, weight loss) and regulate your body’s immune system reaction.
Medication
Depending on the kind of autoimmune disease you have, how severe it is, and how you are feeling, your healthcare provider may recommend several drugs and other treatments. Physicians might also administer blood transfusions if the condition damages your blood. They might use the following medications to suppress an overreaction of the immune system:
Steroids: Because they reduce your immune system’s hyperactive reaction fast and efficiently, a class of medications known as corticosteroids is frequently used as the initial line of treatment. However, these have the potential to cause major negative effects as they weaken your immune system as a whole.
Anti-inflammatory drugs. These drugs support the health of organs while also assisting in immune system regulation. Anti-TNF drugs, for example, combat the protein known as tumor necrosis factor (TNF), which promotes inflammation. They’re utilized for the treatment of autoimmune arthritis in certain ways.